
Blog
With over 30 years nursing experience and 10 of those being in the community with geriatric clients, I will give you the information you need to help an aged loved one.


Benzodiazepines
I have at times struggled with anxiety and depression. The doctors will usually prescribe an SSRI (selective serotonin uptake inhibitors) medication that can be used to treat depression and/or anxiety. At times physicians may also prescribe benzodiazepines like Clonazepam or Xanax. I have avoided using these medications because they are addicting and now research shows that they also can be a risk factor for Alzheimer's.
In this blog post, we'll delve into the world of benzodiazepines, commonly known as benzos, and their impact on the elderly population. These medications can be risky in older individuals and it’s important to know if your care recipient is receiving these medications and for how long.
Benzos, a class of medications that includes Clonazepam, Valium, and Xanax, are often prescribed to alleviate anxiety and sleep-related issues. While they can provide relief, especially for older individuals facing unique challenges like anxiety about health, becoming a burden, or sleep problems, they also come with significant concerns.
One critical factor to consider is benzos' long half-life, which refers to how long it takes for half of the medication to leave the body. In older people, this half-life is even longer due to factors like increased fat distribution, reduced liver and kidney function, and heightened sensitivity to benzos in the brain. The longer these medications stay in a person’s system, they become at risk for sleepiness and falls.
Dependency and addiction to benzos can also be a serious issue, particularly in older adults. These medications can be habit-forming, and an individual might take more to get the same effect. Withdrawal symptoms can be challenging to manage. It's important to approach dependency with caution and seek medical guidance for gradual tapering if needed.
One of the most concerning aspects of long-term benzo use in older individuals is its association with dementia and cognitive decline. Studies have revealed that the risk of dementia increases with age, partly due to the prolonged presence of benzos in the body. This underscores the importance of exploring alternative treatments for anxiety and sleep issues.
In the United States, guidelines have been established to ensure benzos and other psychiatric medications are prescribed only when there's a confirmed psychiatric condition. However, surveys reveal that these guidelines are not always followed in facilities like nursing homes and assisted living communities. In such settings, residents may be prescribed benzos without a clear diagnosis, often to address feelings of isolation and depression.
It's crucial to explore with a care recipient’s primary care manager the need for benzos for older individuals struggling with mental health issues. These can include safer medications and counseling. Depression, in particular, should be assessed carefully, as it can have various causes, including vitamin deficiencies and other medical conditions.
To safeguard the well-being of your elderly loved ones, it's essential to have open and honest conversations about their medications. If you discover that they are taking benzos, inquire about the duration and discuss the potential risks. Encourage them to consult with their healthcare provider to explore alternative treatments or a gradual tapering plan.
While benzos can offer relief for anxiety and sleep problems in older adults, the potential risks, including dependency, addiction, and an increased risk of dementia, must not be underestimated. It's our responsibility to advocate for our loved ones' mental health and well-being, seeking safer and more effective alternatives when possible. By staying informed and fostering open communication, we can help our elderly family members navigate their mental health challenges with care and caution.

Shower Safety Equipment
Title: Ensuring Safety and Comfort: Choosing the Right Shower Chair for Seniors
Falls are a concern among older adults, particularly those over the age of 65, with one in three experiencing a fall each year. Among the places where these accidents occur most frequently is the shower. In this blog, we'll delve deeper into the importance of making showers safer for seniors and provide valuable insights into selecting the right shower chair for their needs.
It's disheartening to witness how falls can drastically impact the lives of older adults. To illustrate this, I shared the experience of my father-in-law, who, after multiple falls, now avoids showers altogether and instead resorts to sponging off. This not only highlights the physical dangers of falling in the shower but also underscores the need for effective solutions.
During my conversations with fellow caregivers and seniors, I've encountered various misconceptions about shower safety. For instance, simply placing a lawn chair, often rusty and unstable, in the shower hardly qualifies as a safe solution. Similarly, a worn-out plastic chair with insufficient weight support can lead to hazardous situations. These types of arrangements are what give nurses and therapists great reflux. Recognizing the need for appropriate equipment and education is vital.
Selecting the Right Shower Chair: When choosing a suitable shower chair, several factors demand careful consideration:
1. Weight Capacity: Always be aware of the chair's weight limit, usually ranging from 200 to 250 pounds. Prioritize safety over cost savings, as inadequate weight support can result in severe injuries. Shower chairs donated through churches and non profits may not be suitable for a heavier person.
2. Back Support: Depending on the individual's needs, decide whether a backrest is necessary. For those capable of sitting upright, a backless chair might suffice. However, individuals with balance issues, like those with Parkinson's, require the added support of a backrest. I usually recommend back supported chairs because they can be used no matter what.
3. Handles and Grip: Chairs with handles offer extra stability and help individuals stand up with ease. While these models might cost slightly more, the added safety and convenience they provide are well worth the investment.
4. Dimensions and Fit: Ensure the chair fits comfortably within the shower or bathtub space. Some individuals might require special adaptations, such as a professional bench installation, to accommodate their unique needs. Benches can sometimes be slippery therefore it is important to put a towel down and make it non skid.
5. Handheld Shower Wand: A handheld shower wand can significantly enhance the shower experience. By allowing users to direct the water flow, adjust the temperature, and avoid direct facial contact with water, this simple addition contributes to both comfort and safety.
6. Bench for Bathtubs: For individuals unable to lift their legs safely over the bathtub's edge, a bathtub bench is a suitable solution. A well-designed bench allows users to sit outside the tub, glide over, and lift their legs into the tub for bathing. Some benches have a gliding chair that will assist an individual to glide over the bathtub edge into the bathrub.
In conclusion, prioritizing shower safety for older adults is paramount. A well-chosen shower chair, tailored to the individual's needs, can significantly reduce the risk of falls and restore a sense of independence. Whether it's a shower chair with adequate weight support, the right backrest, or the convenience of handles and a handheld shower wand, these considerations can make a world of difference.
Remember, the goal is to create an environment where seniors feel confident, secure, and comfortable while maintaining their personal hygiene. By taking these steps, we can ensure that shower time remains a refreshing and enjoyable experience for our loved ones. Always consult a medical professional for personalized advice and recommendations.

The Stress of Caregiving
I sat in the living room as the wife Jane told me about her husband Bob’s disability. “H falls, he has trouble getting his shirt and he stumbles to the bathroom,” she explains. After five minutes she stops and starts to cry and says, “I do not want to put him in a nursing home.”
I rubbed her shoulders and said, “I know this is hard. We would love to bring in caregivers to help you out.”
The next thing I knew she showed me their family’s picture album. I see a smiling family with four children petting a kangaroo at the zoo. We flipped through happier memories. I wish I could have a magic button to travel back in time three years ago when Bob was first starting to need care. The wife thought she could take of her husband by herself without any help. Unfortunately now she is close to having an emotional breakdown due to the stress of caregiving.
Studies show that elderly informal spousal caregivers experience more stress than non-spousal caregivers and this causes more mental and physical health problems. One of the reasons for this is that stress causes an increase in a protein called interleukin-6 (IL-6). Normally, IL-6 elevates in our body in response to an infection. When it goes up due to stress it causes chronic inflammation in our bodies. Individuals with chronic elevated IL-6 experience lowered immunity, dementia, and bone loss.
Scientist divided two groups of elderly individuals. One group were spousal caregivers, and the other group were not caregivers. After drawing their blood, they discovered that spousal caregivers had four times more IL-6 in their blood stream than spouses who were not caregivers. Many spousal caregivers also skip doctor’s appointment because they cannot find the time to prioritize their health. This is one reason spousal caregivers experience more health challenges than non-spousal caregivers.
All is not doom and gloom though for spousal caregivers. Scientist studied spousal caregivers by encouraging one group to eat healthy and a second group to exercise. The spouses who exercised were able to bring down their IL-6. This shows that certain behaviors can mitigate the stress of being a caregiver.
The second thing that helps with stress is to get help for the spousal caregiver. One day my mother-in-law called me to say that her husband had fallen down the steps. As the weeks progressed and I called to check on them I realized my father-in-law was developing dementia. My mother-in-law told me she was nervous to leave her husband alone because his decision making was skewed. As soon as I realized she was becoming a caregiver we worked to get her help as she lived away from her children. I interviewed home care agencies and hired an agency to send a paid caregiver to stay with my father-in-law twice a week. My mother-in-law talked about how having that eight hours to herself greatly lowered her stress.
Unfortunately, I see too many spouses unwilling to ask the family for help or spend their money to get help. Besides the multitude of health problems I have seen develop in spousal caregivers, statistic show that about 30% of spousal caregivers will pass away before the person they are caring for. I constantly remind caregivers that without them their loved one cannot stay home therefore; they must take care of themselves. Practicing self-care is just as important as taking care of our loved one. Self care will help spousal caregivers have healthier and happier lives.
https://www.agingcare.com/discussions/thirty-percent-of-caregivers-die-before-the-people-they-care-for-do-97626.htm#:~:text=Thirty%20Percent%20of%20Caregivers%20Die%20Before%20The%20People%20They%20Care%20For%20Do,-Follow&text=Rough%20statistics%20show%20that%2030,are%20high%20on%20the%20list.
https://www.caregiver.org/resource/caregiver-statistics-demographics/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3839348/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC166443/
https://academic.oup.com/gerontologist/article/56/Suppl_3/69/2576281
https://www.pnas.org/content/117/28/16258
https://cpb-us-e1.wpmucdn.com/blogs.rice.edu/dist/1/4371/files/2015/07/7.The-Chronic-Stress-of-Caregiving-1-1qt0d2z.pdf
https://www.researchgate.net/publication/285945176_The_Chronic_Stress_of_Caregiving_Accelerates_the_Natural_Aging_of_the_Immune_System
https://www.hopkinsmedicine.org/the-academy/_docs/Roth_Academy_Feb2020.pdf
The Inner Ear Matters
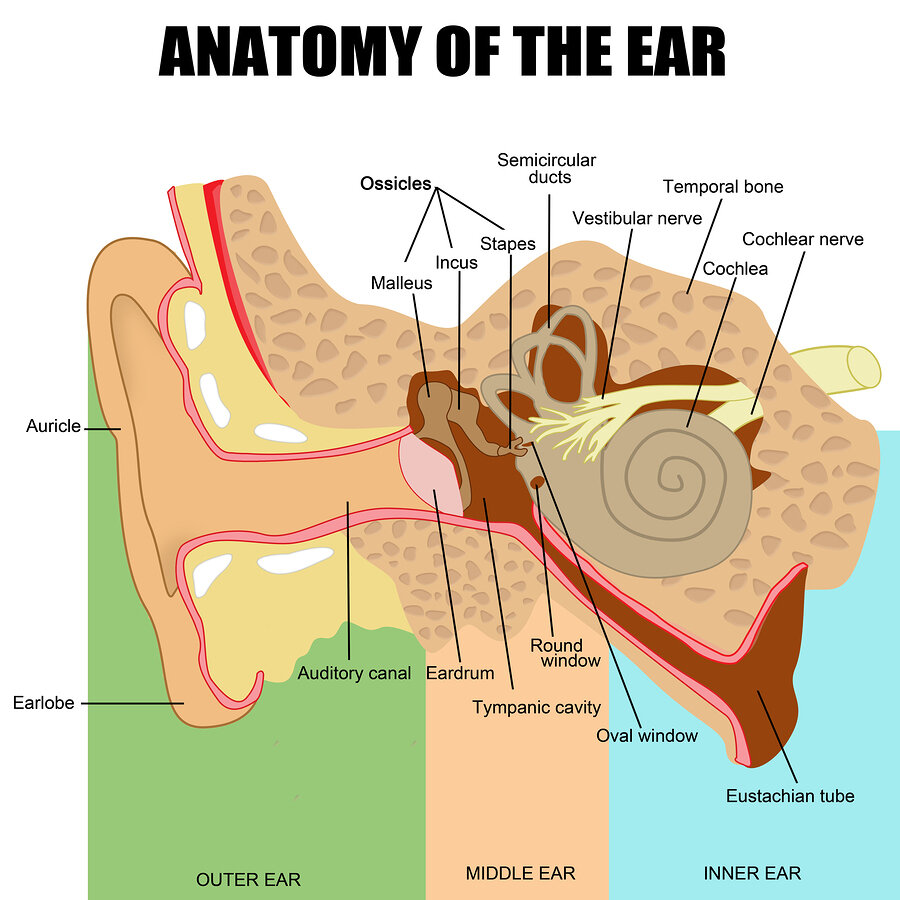
One in three adults over the age of 65 fall every year. Many times, this leads to long hospital stays, disability and long-term care placement. Many reasons exist for why seniors fall, but one reason is problems with their inner ear.
